Giant Aneurysmal Bone Cyst of the Mandibular Condyle Mimicking Parotid Tumor: A Case Report and 22-Year Follow-Up
June 16, 2023
J Diagn Treat Oral Maxillofac Pathol 2023;7: 51–62.
DOI: 10.23999/j.dtomp.2023.6.1
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Dhaif G, Dhaif M, Sethi A. Giant aneurysmal bone cyst of the mandibular condyle mimicking parotid tumor: a case report and 22-year follow-up. J Diagn Treat Oral Maxillofac Pathol 2023;7(6):51–62. https://doi.org/10.23999/j.dtomp.2023.6.1
NATIONAL REPOSITORY OF ACADEMIC TEXTS
https://nrat.ukrintei.ua/en/searchdoc/2023U000250/
ABSTRACT
Background: Aneurysmal bone cyst (ABC) is a rare benign non-odontogenic cyst that occurs most commonly in the posterior mandible. Occurrence in the mandibular condyle is rare. We present a case that was initially misdiagnosed as a parotid gland tumor and later was found to be an ABC.
Case Presentation: A 19-year-old man presents with a painless firm swelling on the right preauricular region. Panoramic imaging revealed a radiolucent lesion in the right condyle and ascending ramus of the mandible with complete erosion of the bony surface losing the condyle configuration. The lesion was excised, and the mandible was curetted. A split-thickness left clavicular joint graft was harvested for reconstruction of the right condyle of the mandible. The pathology report confirmed the diagnosis of aneurysmal bone cyst. The patient was followed for 22 years without any evidence of recurrence.
Conclusions: Tumors of the jaws and cystic lesions may mimic benign salivary gland pathology. Appropriate clinical and radiographic examination should be utilized to exclude this from the differential diagnosis. Complete surgical excision of the lesion and reconstruction of the condyle may be utilized to provide patients with good results.
Keywords: Reconstructive surgical procedures, aneurysmal bone cyst, pseudocyst, benign bone lesions, mandibular condyle.
BACKGROUND
Aneurysmal bone cysts (ABCs) are rare, benign, non-odontogenic cysts, accounting for less than 1% of all non-epithelial cysts in the jaw.1 These cysts typically affect patients aged 10-30 years, with no discernable sex predilection.2 They are more commonly found in the posterior mandible than in the maxilla.3 However, the occurrence of an aneurysmal bone cyst in the mandibular condyle is rare, and the etiology of these cysts remains unknown and enigmatic.4 Although several theories have been proposed, the precise nature of their pathogenesis is still unclear. Aneurysmal bone cysts exhibit a distinct clinical presentation and are generally asymptomatic. In most instances, the lesion appears as an indolent, painless, radiolucent lesion during routine radiographic assessments or after significant bony expansion has occurred.5
In this paper, we present a rare case of an aneurysmal bone cyst in the mandibular condyle, with a 22-year follow-up after surgical intervention and discuss the management challenges that were encountered during the treatment process.
CASE REPORT
A 19-year-old male patient was referred to the Department of Oral and Maxillofacial Surgery at the Salmania Medical Complex in Bahrain by an ear, nose, and throat (ENT) surgeon for evaluation of a mass in the right preauricular region. Initially, the patient was referred from a health center to the ENT Department for assessment of a possible benign parotid tumor. The patient's past medical history was non-contributory. Physical examination revealed a painless, firm swelling in the right preauricular region, significantly stretching the skin, and elevating the right earlobe (Fig 1). Facial nerve functions were preserved, and no palpable lymph nodes were detected in the face or neck. Maximum mouth opening was within normal limits, but deviation of the mandible to the left side occurred upon opening. There was no clicking or locking of the temporomandibular joint (TMJ).
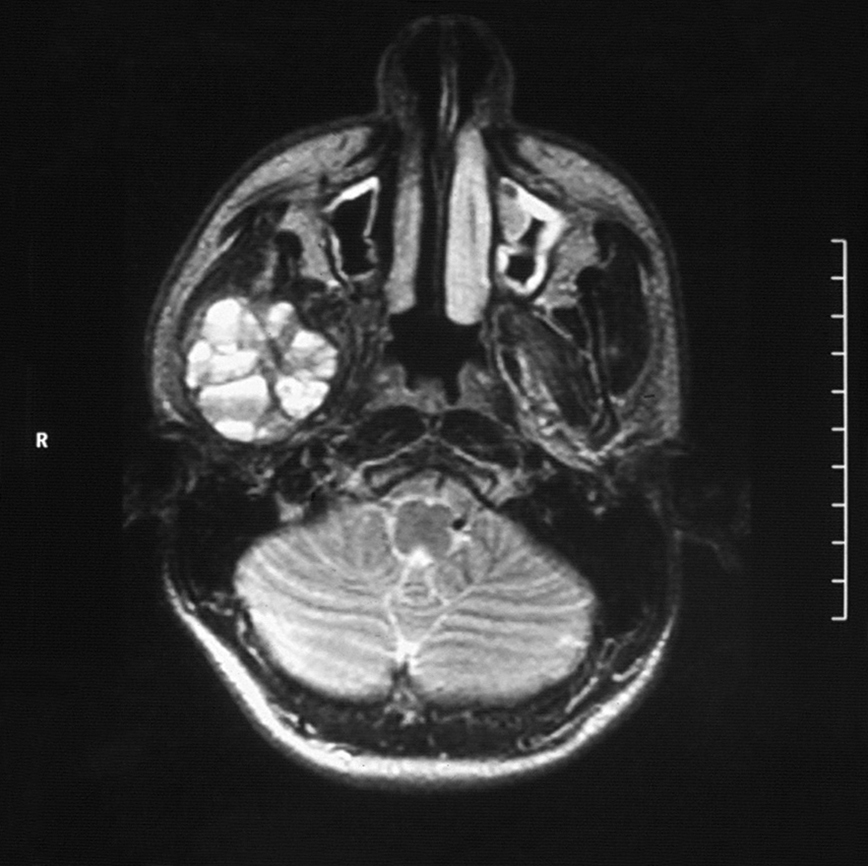
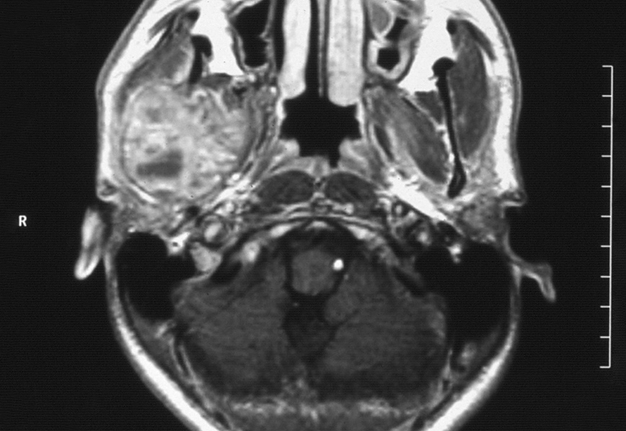
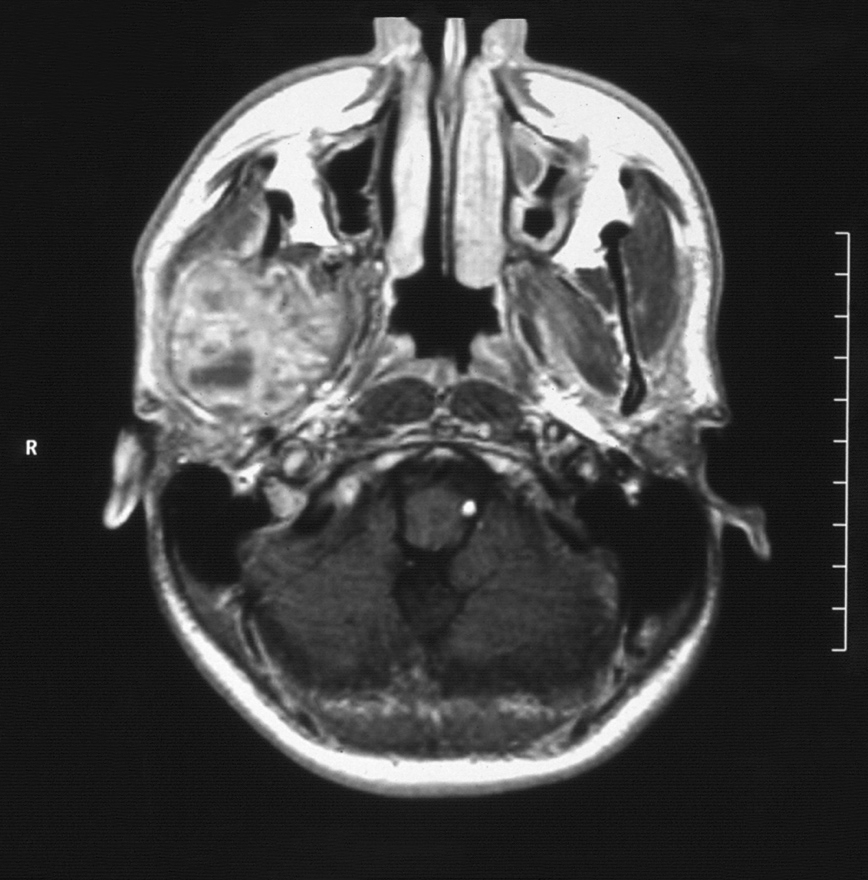
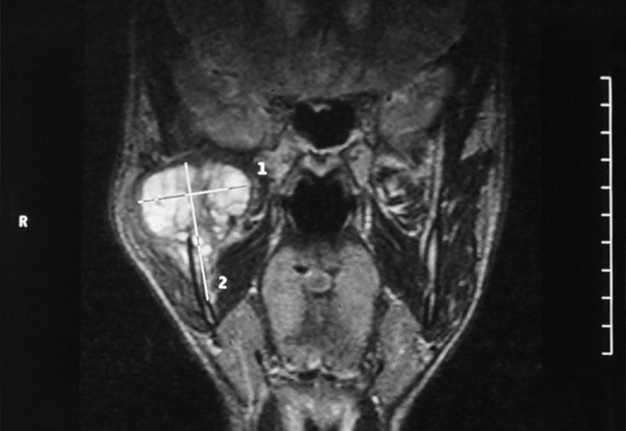
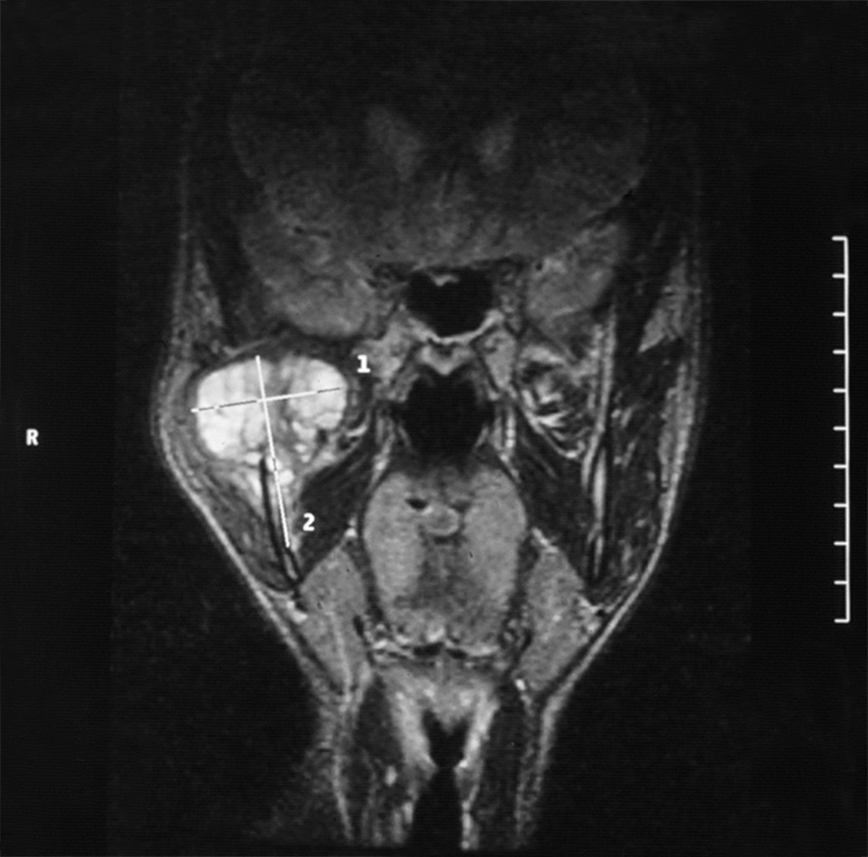
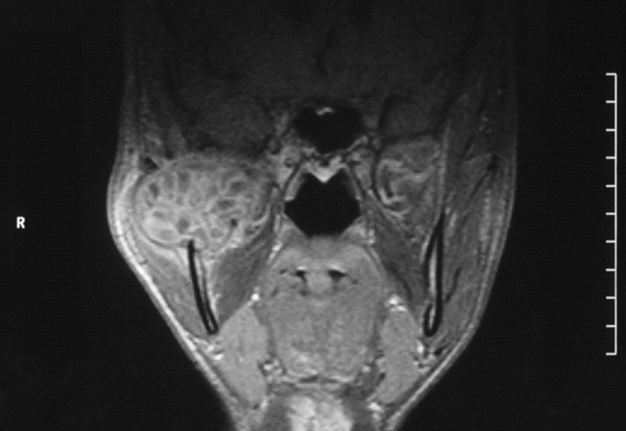
Intraorally, the parotid duct appeared normal in color, with normal salivary flow and no evidence of pus discharge. The patient did not recall any history of trauma to the region or any recent dental procedures. A plain radiograph of the skull showed no evidence of stones or calcifications in the right parotid gland. The magnetic resonance imaging (MRI) of the head and neck region revealed a normal parotid gland with no evidence of any pathology in the gland or its surrounding tissues. However, there was a large destructive mixed radiopaque/radiolucent on the right mandibular condyle extending superiorly and encroaching on the skull base, and posterosuperiorly invading the infratemporal region (Fig 2). There were multiple calcifications in the lumen of the lesion (Fig 3).
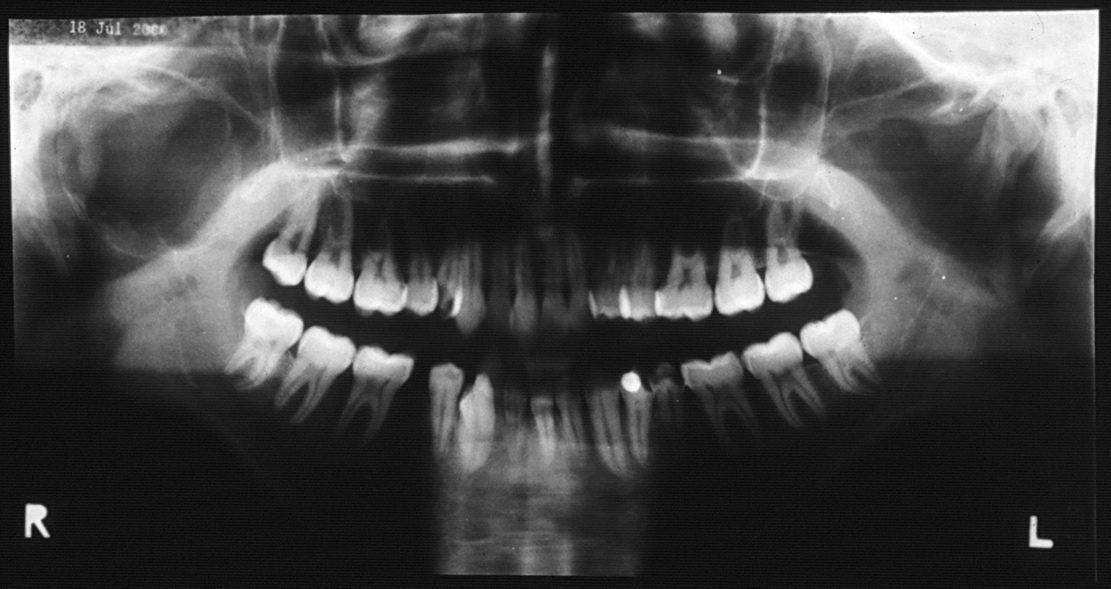
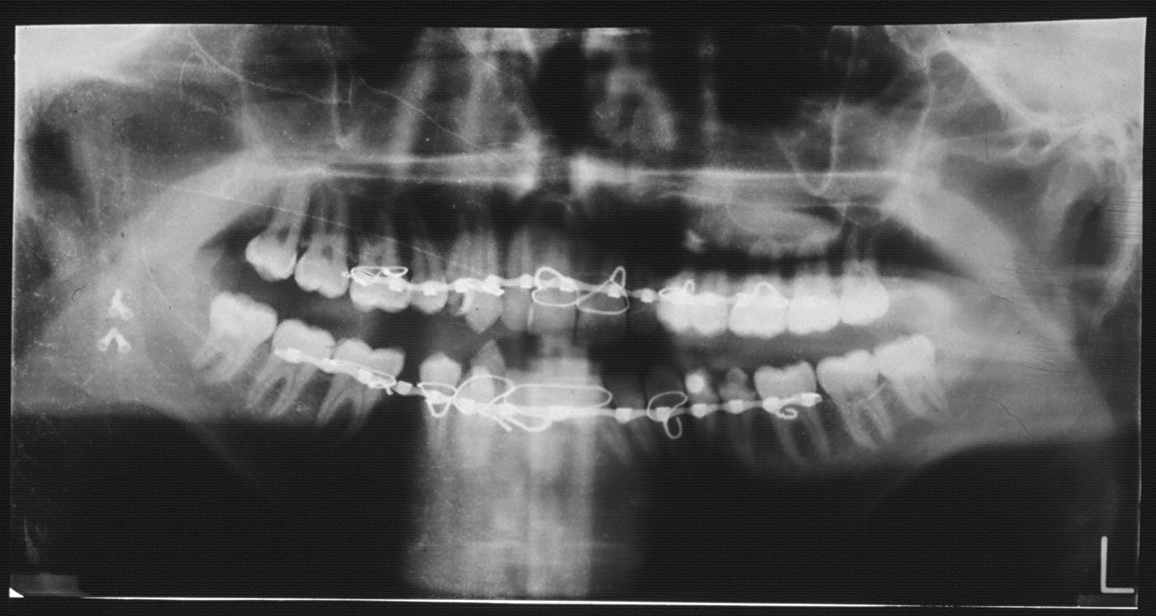
These findings did not suggest parotid gland pathology but rather a tumor or cystic lesion of the jaws. The patient was subsequently referred to our department for further investigation and management. Panoramic radiograph revealed a radiolucent lesion in the right condyle and ascending ramus of the mandible, with complete erosion of the bony surface, resulting in the loss of condylar configuration (Fig 4). The lesion displayed a poorly defined scalloped border and extended inferiorly to the inferior dental foramen. The coronoid process could not be visualized from this view, giving the illusion of erosion by the lesion. However, no paresthesia was noted along the distribution of the inferior alveolar nerve or its terminal branch. Aspiration yielded dark straw-colored fluid mixed with blood. Routine blood investigations, including complete blood count, erythrocyte sedimentation rate, differential white blood count, serum calcium, phosphorus, and alkaline phosphatase, were all within normal limits. Differential diagnoses for this case included simple bone cyst, traumatic bone cyst, aneurysmal bone cyst, calcifying odontogenic cyst, adenomatoid odontogenic tumor, central giant cell granuloma, or ameloblastoma.
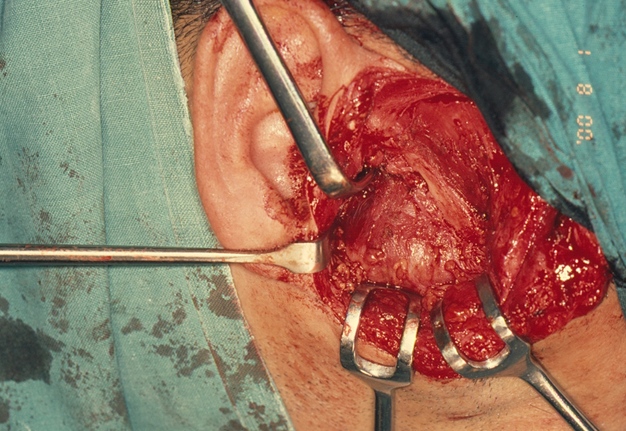
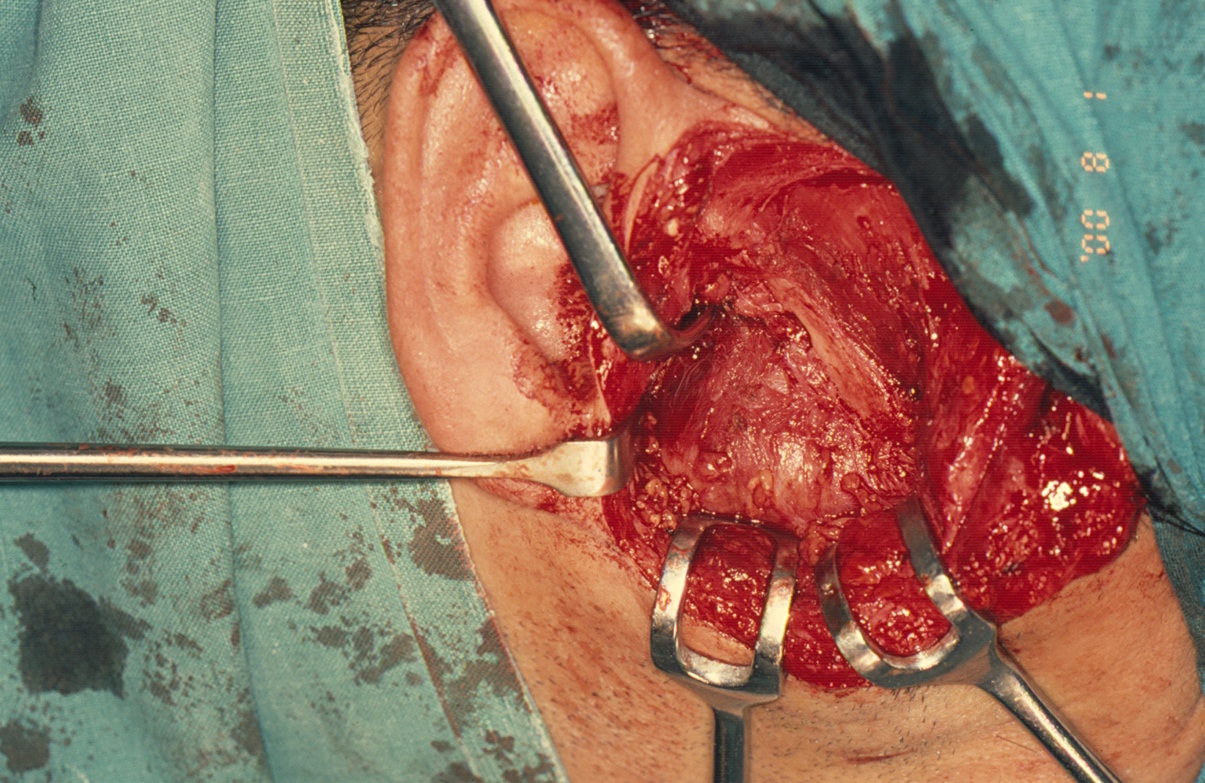
Under general anesthesia, a right preauricular incision with temporal extension was made (Fig 5). The zygomatic arch, condylar fossa, and ascending ramus on the right side were identified. A soft, brown, and vascular mass was observed, stretching the capsule of the right TMJ. The mass measured approximately 10 × 8 × 7 cm. The bone was completely eroded up to the junction between the right angle of the mandible and ascending ramus. Medially, it was difficult to ascertain the exact extent of the mass. The mass was carefully dissected from the surrounding normal tissues. Extensive bleeding from the maxillary artery, encompassed by the mass, was encountered. The artery was identified and ligated. The remaining part of the mandible was curetted to ensure complete excision of the lesion. The articular disc of the right TMJ was absent, and the articular fossa was significantly thinned due to pressure resorption.
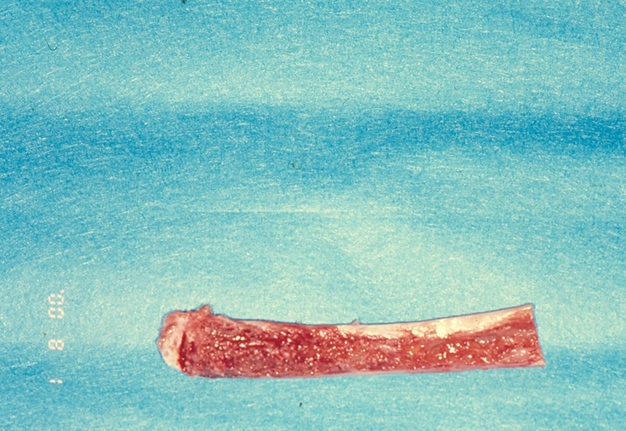
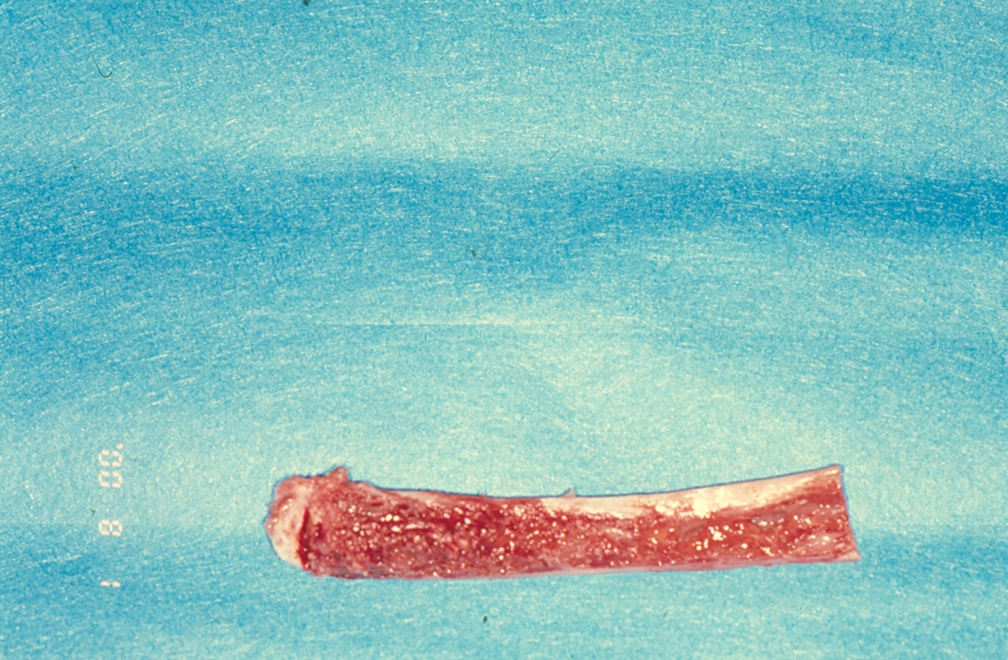
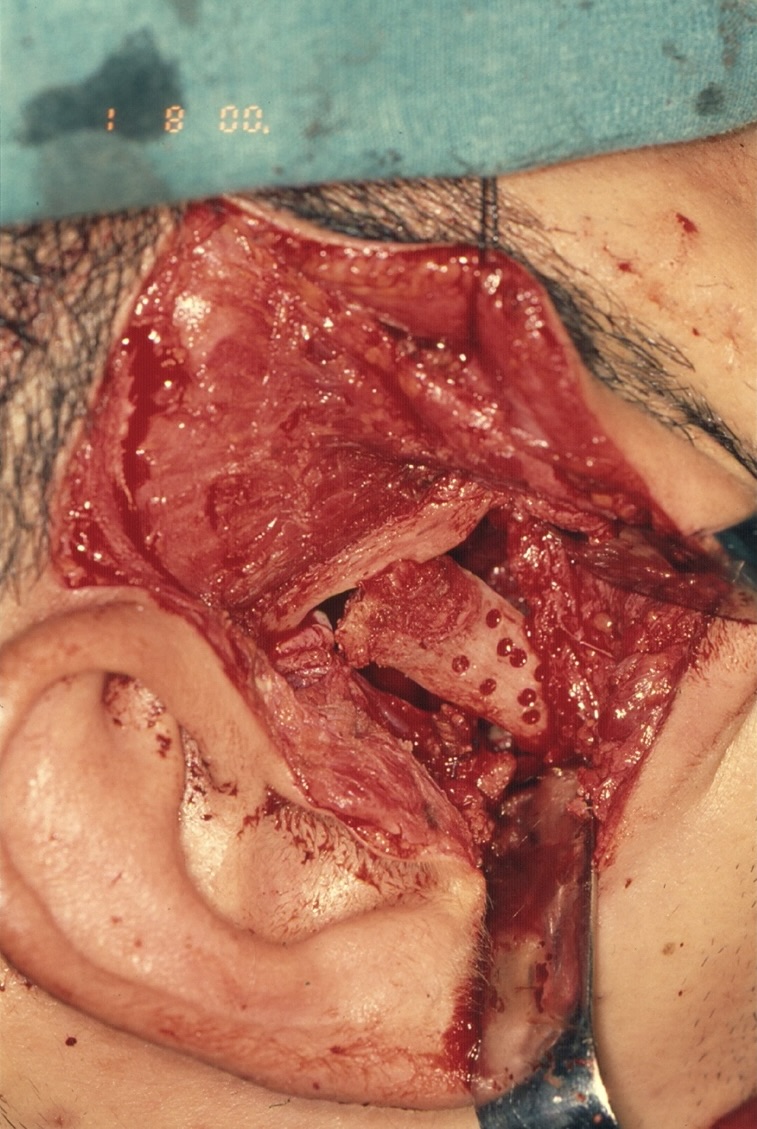
A sternoclavicular joint graft closely resembles the TMJ both morphologically and histologically, as both joints are covered in fibrocartilage. Although costochondral grafts continue to be used for TMJ reconstruction, they are associated with unpredictable growth, warpage, and potential for fracture.6 Consequently, a split-thickness left clavicular joint graft was harvested to reconstruct the right mandibular condyle (Fig 6). To ensure vascularization, the graft was perforated and secured using four 20-mm (KLS Martin, Tuttlingen, Germany) bone screws (Fig 7).
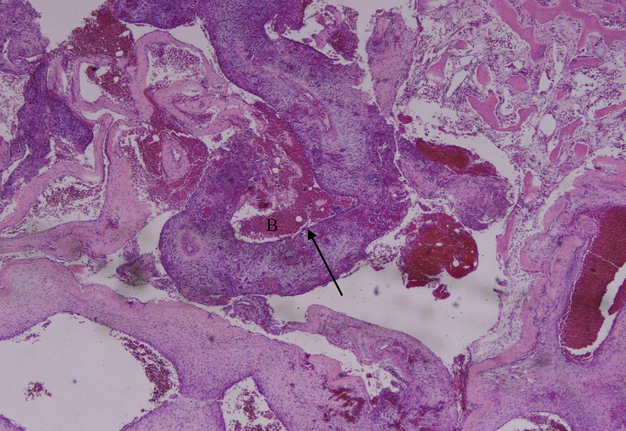
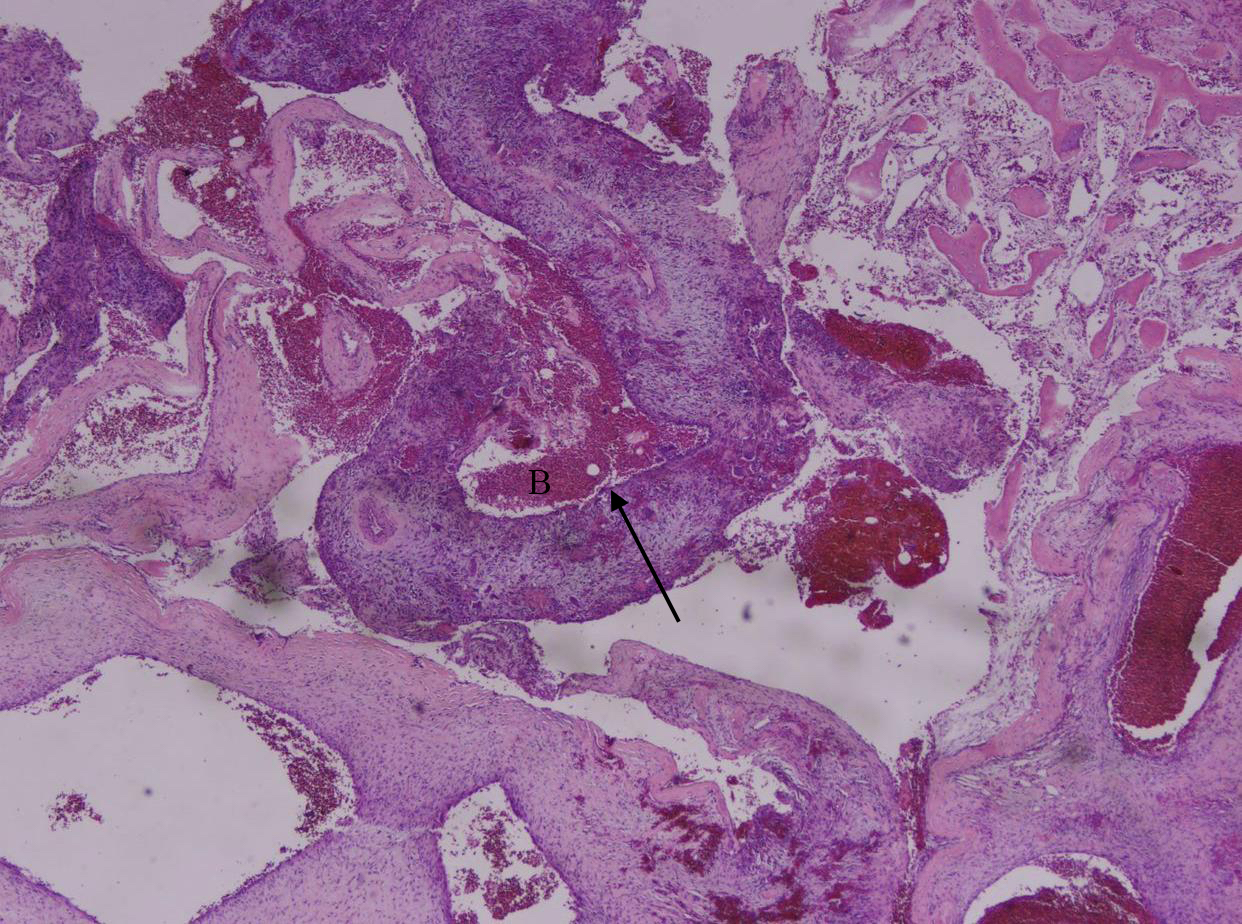
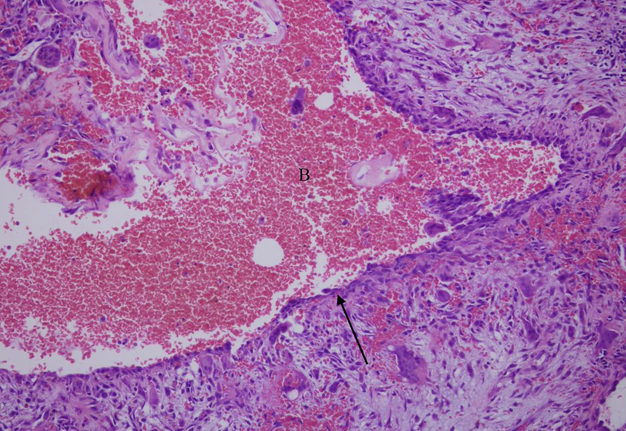
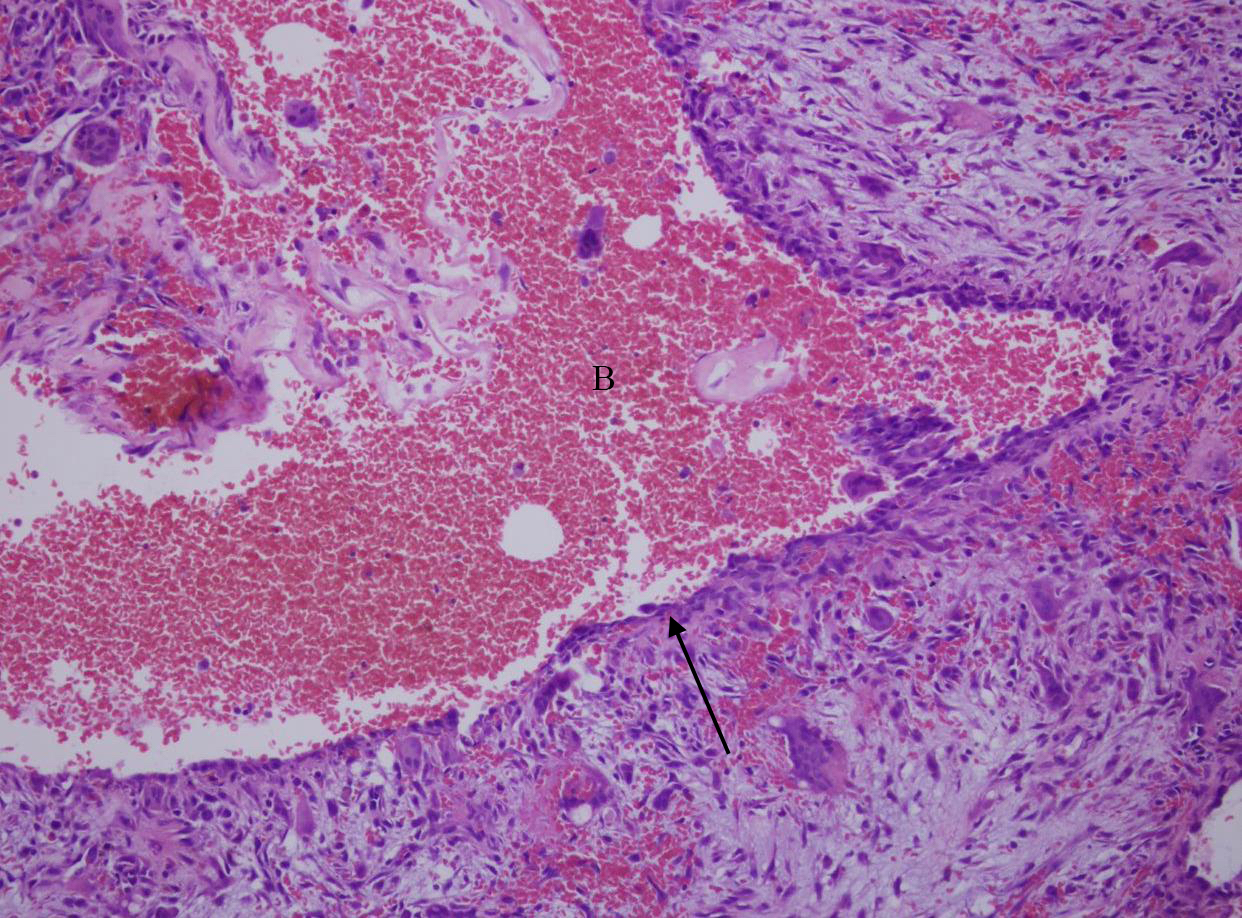
Postoperative care for the patient entailed arch bar placement with elastics for six weeks, during which the patient was instructed to maintain a soft diet. At the six-week follow-up, the arch bars were removed, and examination revealed good mouth opening. A routine postoperative panoramic radiograph demonstrated stable fixation of the right clavicular joint (Fig 8). The final pathology report confirmed the diagnosis of an aneurysmal bone cyst (Fig 9).
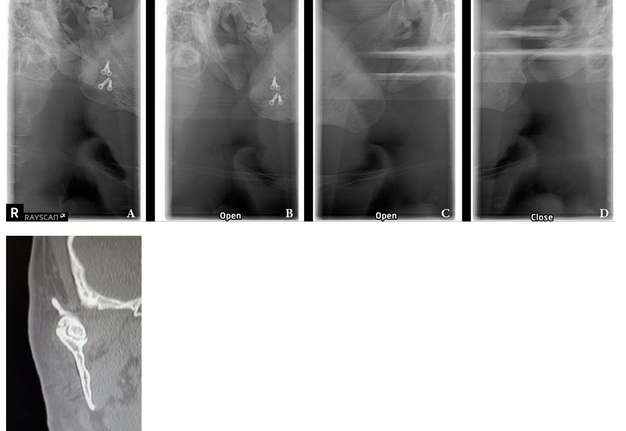
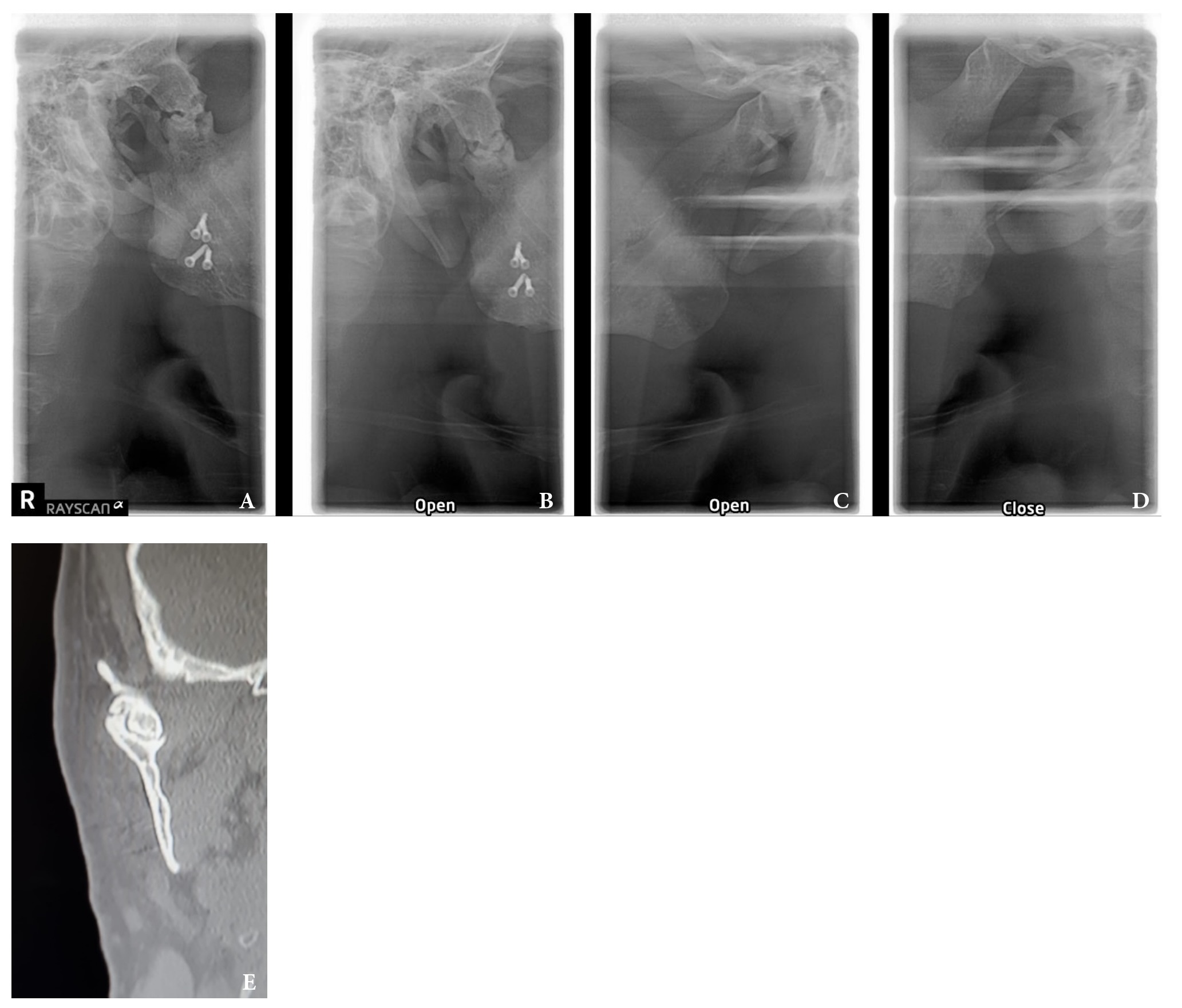
Over a 22-year follow-up period, no signs of recurrence were observed (Fig 10). Furthermore, facial symmetry and normal joint function were successfully restored (Fig 11). At the 22-year follow-up post-surgery, fragmentation was noted in the affected right condylar head (Fig 12), which subsequently healed normally. Possible contributing factors for this development include the extended duration of follow-up, the patient's loss of posterior teeth, and subsequent joint overloading. This is also a recognized drawback of utilizing the sternoclavicular joint for TMJ reconstruction.
FIGURE 12. Imaging during closed and open mouth position on 22-year follow-up. A: Radiograph of the right TMJ with the mouth closed; B: Radiograph of the right TMJ with the mouth open; C: Radiograph of the left TMJ with the mouth open; D: Radiograph of the left TMJ with the mouth closed; E: Coronal computed tomography scan with the mouth closed.
DISCUSSION
The ABC remains enigmatic, with its origin still obscure and the precise pathological nature yet to be determined.1 Although considered a non-odontogenic epithelial cyst, it is not a true bone cyst.2 ABCs are more commonly found in long bones or vertebral columns, rather than in the jaws.3
The etiology and pathogenesis of aneurysmal bone cysts are not fully understood, and there is debate as to whether they arise de novo or result from a vascular accident in a pre-existing lesion.4 Some propose that the development of ABCs may occur in a pre-existing intra-bony lesion due to a dilated vessel.4 Others argue that the transformation of a primary lesion, such as central giant cell granuloma or fibrous dysplasia, into an aneurysmal bone cyst may be initiated by microcysts. These microcysts may then enlarge and coalesce, causing rupture of adjacent vasculature.5 Subsequently, an increase in intracystic pressure and bone resorption would follow in the cascade process, making ABCs a secondary phenomenon.
Most reported cases involve patients younger than 30 years old, with a higher prevalence among females.5 ABCs are more common in the mandible, particularly in the molar region.
The clinical presentation of patients with aneurysmal bone cysts is remarkably variable. However, patients typically present with a painless, firm, or hard facial swelling that is insidious in onset.7 This swelling often results from the perforation of the outer cortex of the bone and subsequent protrusion into the surrounding soft tissue.8
In some cases, ABCs may be detected during routine radiographic assessments of teeth or adjacent structures. Tooth mobility is uncommon, and teeth generally retain their vitality.9
The radiographic appearance of the aneurysmal bone cyst is variable and nonspecific. Several descriptions have been described in the literature depending on the amount of bony destruction and perforation of the bony cortex and periosteal reaction. ABCs can manifest as either unilocular or multilocular radiolucencies associated with discernible cortical expansion and thinning. They are often characterized by a soap-bubble or moth-eaten appearance, and sometimes a sclerotic border is quite evident as a result of new reactive bone formation.2
Radiographic assessment of ABCs is crucial for proper preoperative evaluation, surgical planning, and determination of lesion extensiveness. Panoramic radiographs, posteroanterior (PA) views of the jaws, computerized tomography, and MRI are all essential, depending on the location, degree of bony lesion, and associated involvement of soft tissues.
The microscopic appearance of ABCs is characterized by spaces of varying sizes filled with blood and surrounded by bland fibroblast/myofibroblast-like spindle cells (Fig 9). A noticeable presence of multinucleated giant cells can be observed in these tissues.11 Although this is pathognomonic of ABCs, microscopic examination should always be complemented by thorough clinical and radiographic assessments.
Various treatment options have been proposed in the literature, including enucleation, curettage, marsupialization, and bone resection. Conservative treatment is typically undertaken for smaller lesions to minimize surgical risks and morbidity. However, larger lesions with evidence of soft tissue involvement should be addressed through en-bloc resection and immediate reconstruction to prevent recurrence and the need for secondary surgical intervention.
Recurrence rates reported in the literature vary depending on the treatment option employed, with rates as high as 50%.12 Regular monitoring of the lesion is crucial to enable early intervention in the event of a recurrence. Consequently, every effort should be made to ensure complete resection with an adequate safety margin.
CONCLUSIONS
In the case we present, the patient exhibited a preauricular painless swelling initially believed to be a parotid tumor. However, MRI ruled out this provisional diagnosis. Consequently, it is essential to recognize that tumors of the jaws and cystic lesions may mimic benign salivary gland pathology. Every effort should be made to exclude this possibility through comprehensive clinical and appropriate radiographic examinations.13
ETHICS APPROVAL
Not applicable.
CONSENT
Written informed consent was obtained from the patient for publication of this report and accompanying images.
COMPETING INTERESTS
Authors declare that they have no competing interests.
AVAILABILITY OF DATA AND MATERIALS
Data sharing is not applicable to this article since no dataset was generated or analyzed during the current study.
FUNDING
This work was carried out without funding support.
AUTHORS’ CONTRIBUTIONS
All the authors contributed to the work described in the paper. GD was the operator of this case and conceived of the study. MD and AS drafted the manuscript. AS contributed to critical revising. All authors read and approved the final manuscript.
ACKNOWLEDGEMENTS
Not applicable.
REFERENCES (13)
-
Park W, Nam W, Park H, Kim HJ. Intraosseous lesion in mandibular condyle mimicking temporomandibular disorders: report of 3 cases. J Orofac Pain 2008;22(1):65–70.
-
Warner BF, Luna MA, Robert Newland T. Temporomandibular joint neoplasms and pseudotumors. Adv Anat Pathol 2000;7(6):365–81. https://doi.org/10.1097/00125480-200007060-00004
-
Waldron CA. Fibro-osseous lesions of the jaws. J Oral Maxillofac Surg 1993;51(8):828–35. https://doi.org/10.1016/s0278-2391(10)80097-7
-
Rapidis AD, Vallianatou D, Apostolidis C, Lagogiannis G. Large lytic lesion of the ascending ramus, the condyle, and the infratemporal region. J Oral Maxillofac Surg 2004;62(8):996–1001. https://doi.org/10.1016/j.joms.2004.04.009
-
Struthers PJ, Shear M. Aneurysmal bone cyst of the jaws. (I). Clinicopathological features. Int J Oral Surg1984;13(2):85–91. https://doi.org/10.1016/s0300-9785(84)80077-0
-
Wolford LM, Cottrell DA, Henry C. Sternoclavicular grafts for temporomandibular joint reconstruction. J Oral Maxillofac Surg 1994;52(2):119–29. https://doi.org/10.1016/0278-2391(94)90391-3
-
Struthers PJ, Shear M. Aneurysmal bone cyst of the jaws. (II). Pathogenesis. Int J Oral Surg 1984;13(2):92–100. https://doi.org/10.1016/s0300-9785(84)80078-2
-
Motamedi MHK. Destructive aneurysmal bone cyst of the mandibular condyle: Report of a case and review of the literature. J Oral Maxillofac Surg 2002;60(11):1357–61. https://doi.org/10.1053/joms.2002.35744
-
Telfer MR, Jones GM, Pell GM, Eveson JW. Primary bone cyst of the mandibular condyle. Br J Oral Maxillofac Surg 1990;28(5):340–3. https://doi.org/10.1016/0266-4356(90)90112-x
-
Gadre KS, Zubahy RA. Aneurysmal bone cyst of the mandibular condyle: Report of a case. J Oral Maxillofac Surg 2000;58(4):439–43. https://doi.org/10.1016/s0278-2391(00)90932-7
-
Lee J, Huang H. Soft tissue special issue: giant cell-rich lesions of the head and neck region. Head Neck Pathol2020;14(1):97–108. https://doi.org/10.1007%2Fs12105-019-01086-2
-
Mankin HJ, Hornicek FJ, Ortiz-Cruz E, et al. Aneurysmal bone cyst: a review of 150 patients. J Clin Oncol2005;23(27):6756–62. https://doi.org/10.1200/jco.2005.15.255
-
Toljanic JA, Lechewski E, Huvos AG, et al. Aneurysmal bone cysts of the jaws: a case study and review of the literature. Oral Surg Oral Med Oral Pathol 1987;64(1):72–7. https://doi.org/10.1016/0030-4220(87)90119-8