Partially Edentulous Arches and Bilateral Mandibular Fracture: Application of Condensation-Silicone Bite Block-Splint, Mandibulo-Maxillary Fixation Screws, and Elastics for Intraoral Immobilization
March 31, 2024
J Diagn Treat Oral Maxillofac Pathol 2024;8: 20–32.
DOI: 10.23999/j.dtomp.2024.3.1
Under a Creative Commons license
HOW TO CITE THIS ARTICLE
Fesenko II, Rybak VA, Mastakov OY. Partially edentulous arches and bilateral mandibular fracture: application of intermaxillary condensation-silicone bite block-splint, mandibulo-maxillary fixation screws, and elastics for intraoral immobilization. J Diagn Treat Oral Maxillofac Pathol 2024;8(3):20–32. https://doi.org/10.23999/j.dtomp.2024.3.1
National Repository of Academic Texts
https://nrat.ukrintei.ua/en/searchdoc/2024U000041/ (in English). https://nrat.ukrintei.ua/searchdoc/2024U000041/ (in Ukrainian)
ABSTRACT. ABSTRACT IN UKRAINIAN (PDF).
Each mandibular fracture is unique. It requires individual treatment solutions due to different number of fracture sites, fracture terms, level of dislocation, presence/absence of the infection, number, location, and condition of teeth, etc. Management of jaw fractures in partially edentulous arches are even more complicated and typically can involve assistance of a dental technician. Published English language literature lacks information about application of condensation silicone (C-silicone) bite block-splint with mandibulo-maxillary fixation (MMF) screws and elastics for management of bilateral mandibular fracture. This is why we present this novel technique developed by our team based on fracture treatment in a 38-year-old male partially edentulous patient. Also, we introduce a Kyiv’s Modification of the Kennedy Classification System of the partially edentulous arches useful for mandible fracture cases. The Kennedy–Kyiv Classification System considers the non-treated teeth roots as supporting locking points (temporary additional retention points) that increase the stability of the bite block-splint and decrease probability of micromovements. Moreover, it contraindicates extracting such teeth roots immediately before the block-splint fixation as extraction of such roots can provoke the alveolar osteitis upon the fracture site(s) healing and immobilization period what will increase the risk of the block removal for the treatment of osteitis. A review of published MMF techniques and appliances designed for mandible fracture treatment is performed. Multiple appliances for partially and totally edentulous mandibles are considered as well as for the dentulous jaws. The Gunning-type splints and its modifications were considered. An in-chair fabrication of C-silicone bite block-splint and its combined application with MMF screws and elastics is a novel alternative for the Gunning splint. This appliance allows to decrease the time typically required for the Gunning splints fabrication, decreases number of the involved specialists, decreases cost of treatment, and easy for performance.
KEY WORDS
Condensation silicone (C-silicone), C-silicone bite block-splint, mandibulo-maxillary fixation (MMF) screws, osteosynthesis, Gunning splint, intermaxillary silicone block, supporting locking points, temporary additional retention points
Section Editor, Trauma: Paul Coulthard, Queen Mary University of London, United Kingdom. Handling Editor and Reviewer A: Oleksandr Drots, Chornomorsk Stomatological Polyclinic, Ukraine. Reviewers B and C: Artur Kuchynskyi, Kyiv City Clinical Hospital No. 12, Ukraine and Zinaida Zhehulovych, Bogomolets National Medical University, Ukraine.
INTRODUCTION
Condensation silicone (С-silicone) impression materials are widely used by dentists for different types of dental purposes (Khan and colleagues, 2020).1 Nevertheless, there are no data in the literature on the use of one of these two impression materials for the fabrication of the bite block-splint that would serve in combination with mandibulo-maxillary fixation (MMF) screws and elastics to immobilize the partially edentulous fractured mandible. In essence, such C-silicone monoblock can be named as a novel modification of the splint developed by Thomas Brian Gunnning (1868) and which is more known as Gunning splint.2 It was described as vulcanite splint enclosing the maxillary teeth in addition to fitting the teeth of the mandible (Fraser-Moodie, 1969).3 Gunning splint is used for intermaxillary fixation of the mandible in partially or totally edentulous mandible cases.
Multiple modifications of the Gunning splint are reported. Shah and colleagues (2018) highlighted modified Gunning splint for the partially edentulous mandible.4 Sharma and colleagues (2020) published detailed modern description of the Gunning splint with embedded Erich’s arch bars for the edentulous mandibles.5 Chaudhary and colleagues (2014) applied MMF screws in combination with Gunning splint and Erich’s arch bars in partially edentulous scenario.6 Authors made intraosseous insertion of the screws through the Gunning splint.6
In this article, we describe a novel technique we applied to several patients with partially edentulous arches upon the mandibular fractures. The paper documents and illustrates one of these cases. We demonstrate a combination of the open reduction internal fixation and conservative treatment of bilateral mandible fracture in partially edentulous patient with nonexistent occlusion. To our knowledge, it is a first report of combined application of intermaxillary C-silicone bite block-splint, MMF screws, and elastics for intraoral immobilization.
CASE REPORT AND TECHNIQUE
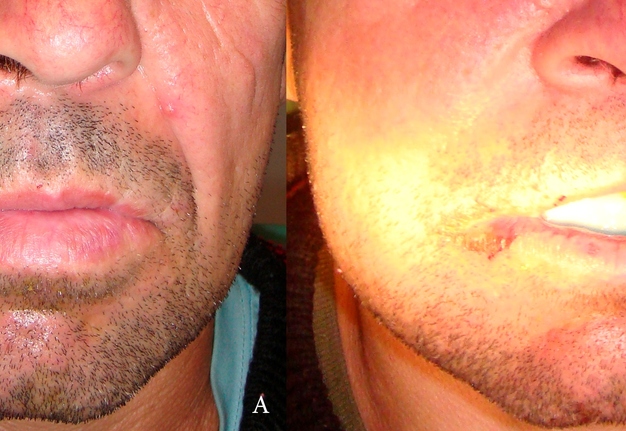
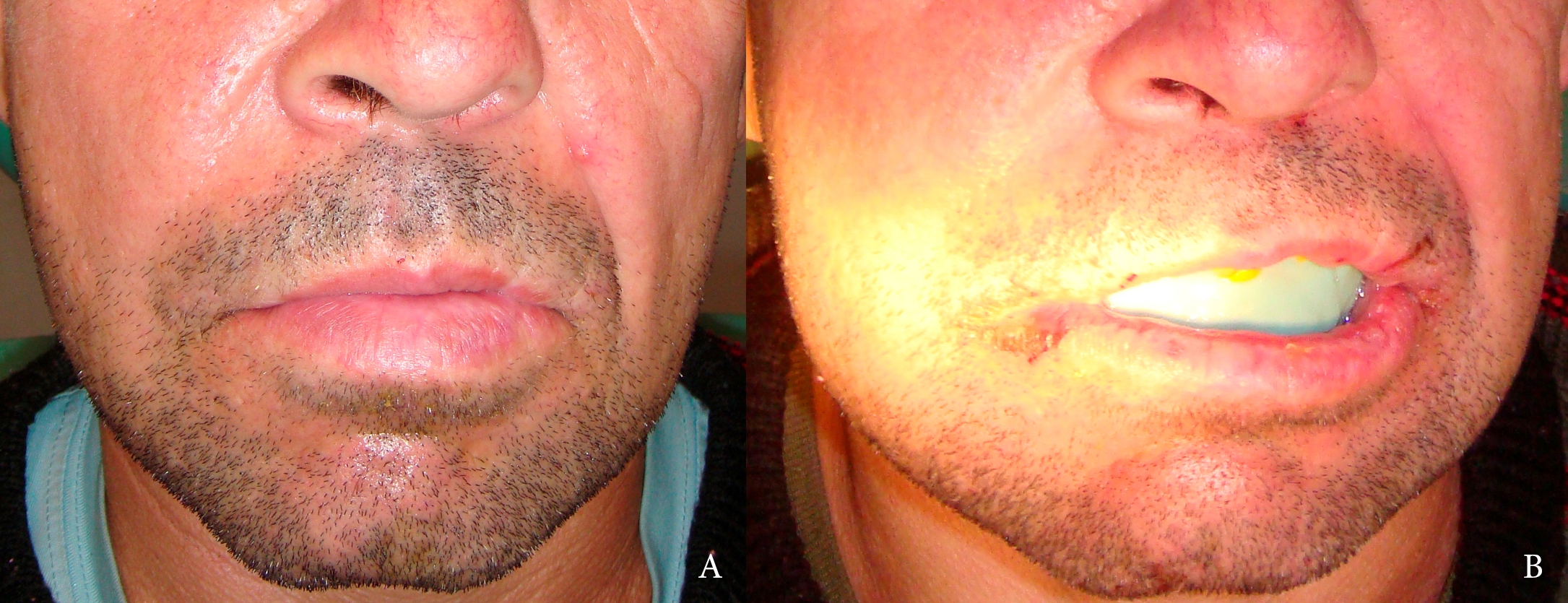
In September 2012, a 38-year-old male patient was referred to the Department of Maxillofacial Surgery, Kyiv Regional Clinical Hospital with a history of a mandible pain and limited mouth opening (Fig 1) after the facial trauma happened several days ago.
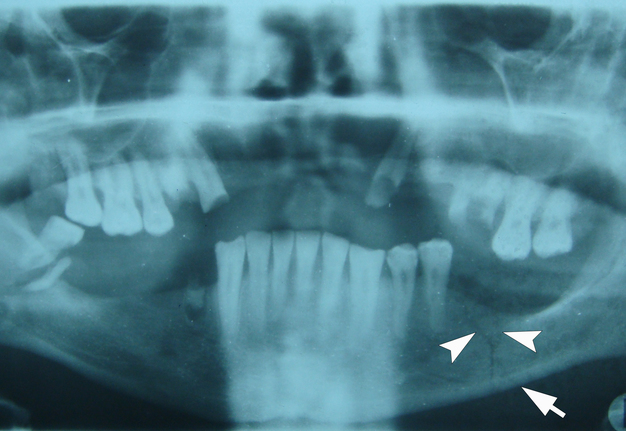
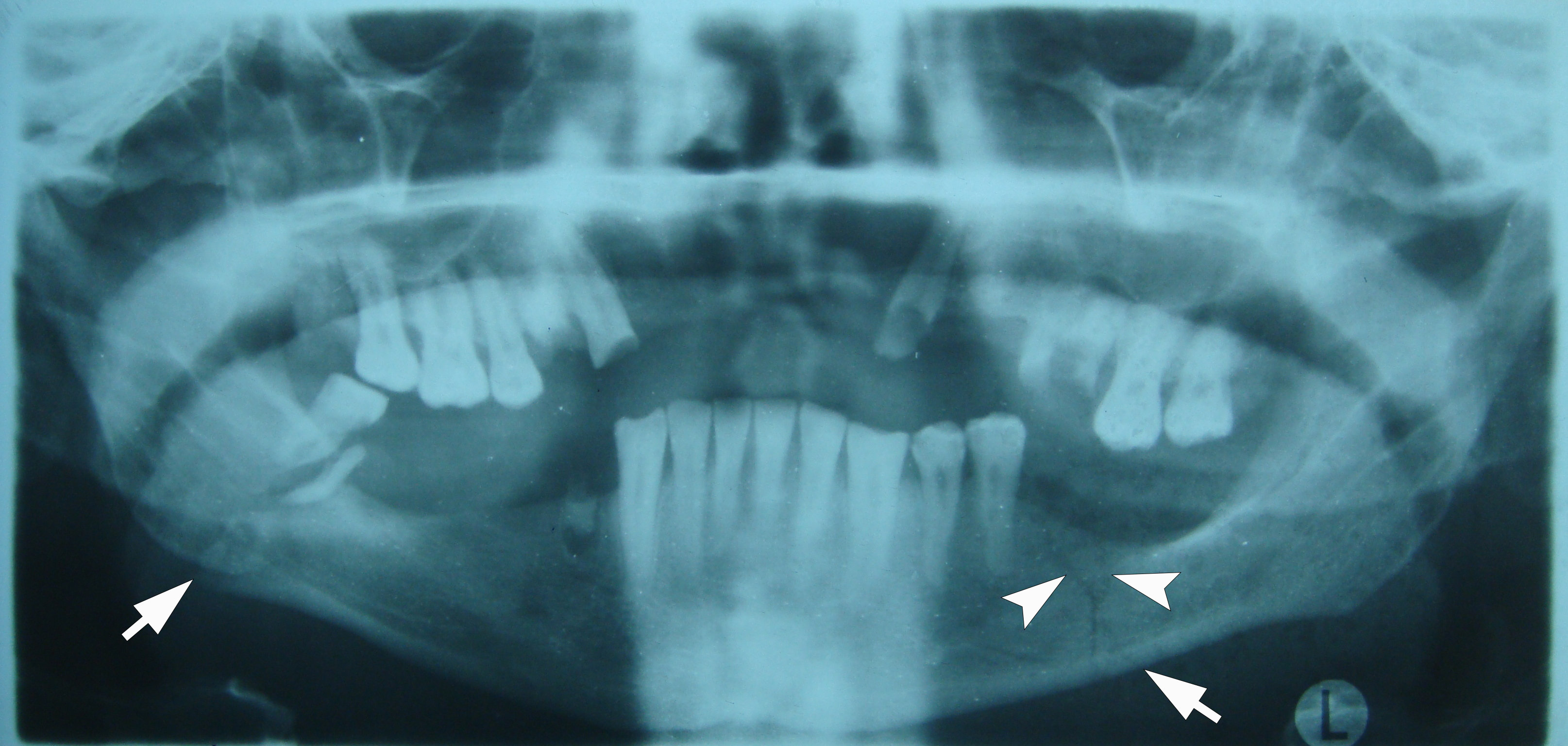
A conventional panoramic radiography (Fig 2) and radiography in anterior-posterior view showed bilateral mandible fracture. The fracture of the left mandibular body without dislocation and fracture of the right mandibular angle with dislocation were noted. Also, the fractured parts of the lower right third molar (i.e., tooth no. 48) were visualized on x-ray.
FIGURE 2. Panoramic radiography shows bilateral mandible fracture (arrows) in a 38-year-old male. Notes fracture of the left mandibular body without dislocation and fracture of the right mandibular angle with dislocation. Also, notes the fractured parts of the lower right third molar. Radiological sign of duplication is indicated by arrowheads.7 L, left side. Printed with permission and copyrights retained by I.I.F.
The bilateral fracture in this case belongs to Kazanjian and Converse Class II, when teeth are present only on one side of the fracture line (Passi and colleagues, 2017).8 The patient had partially edentulous arches and missing occlusion (Fig 3). So, according to FLOATIS classification of mandibular fracture, nonexistent occlusion (O0) was established.8 Also, it was established Kennedy Class IV (or Kennedy-Kyiv Class IV) on the upper jaw and Kennedy Class I (or Kennedy-Kyiv Class I) on the lower jaw (Şakar, 2016).9 Upon the establishment classes of the partially edentulous jaws, we proposed a Kyiv’s Modification of the Kennedy Classification System of the partially edentulous arches (Kennedy–Kyiv Classification System). According to the rules which have been provided by Applegate to govern application of the Kennedy classification (Şakar, 2016),9 the classification should follow rather than precede extraction (classification is identified after extraction[s]). Nevertheless, the roots of the teeth are considered in the Kennedy–Kyiv Classification, because (1) they are supporting locking points (i.e., temporary additional retention points) that increase the stability of the intermaxillary silicone bite block-splint described below and (2) extraction of such roots can provoke the alveolar osteitis upon the fracture site(s) healing and immobilization period what will increase the risk of the block removal for the treatment of osteitis.
FIGURE 3. Pretreatment intraoral view of the upper (A) and lower (B) jaw. The roots of the teeth no. 1.5, 1.4, 2.3, and 4.4 act in this situation as additional temporary anti-rotation points of fixation for the intermaxillary C-silicone bite block-splint. Printed with permission and copyrights retained by I.I.F.
It was decided to remove the tooth fragments in the fracture gap, to perform open reduction internal fixation of the right mandible, insertion of MMF screws for intraoral immobilization, and to produce a silicone bite block-splint to make intermaxillary fixation possible. Antibiotic therapy was started immediately after the diagnosis and lasted for 7 days.
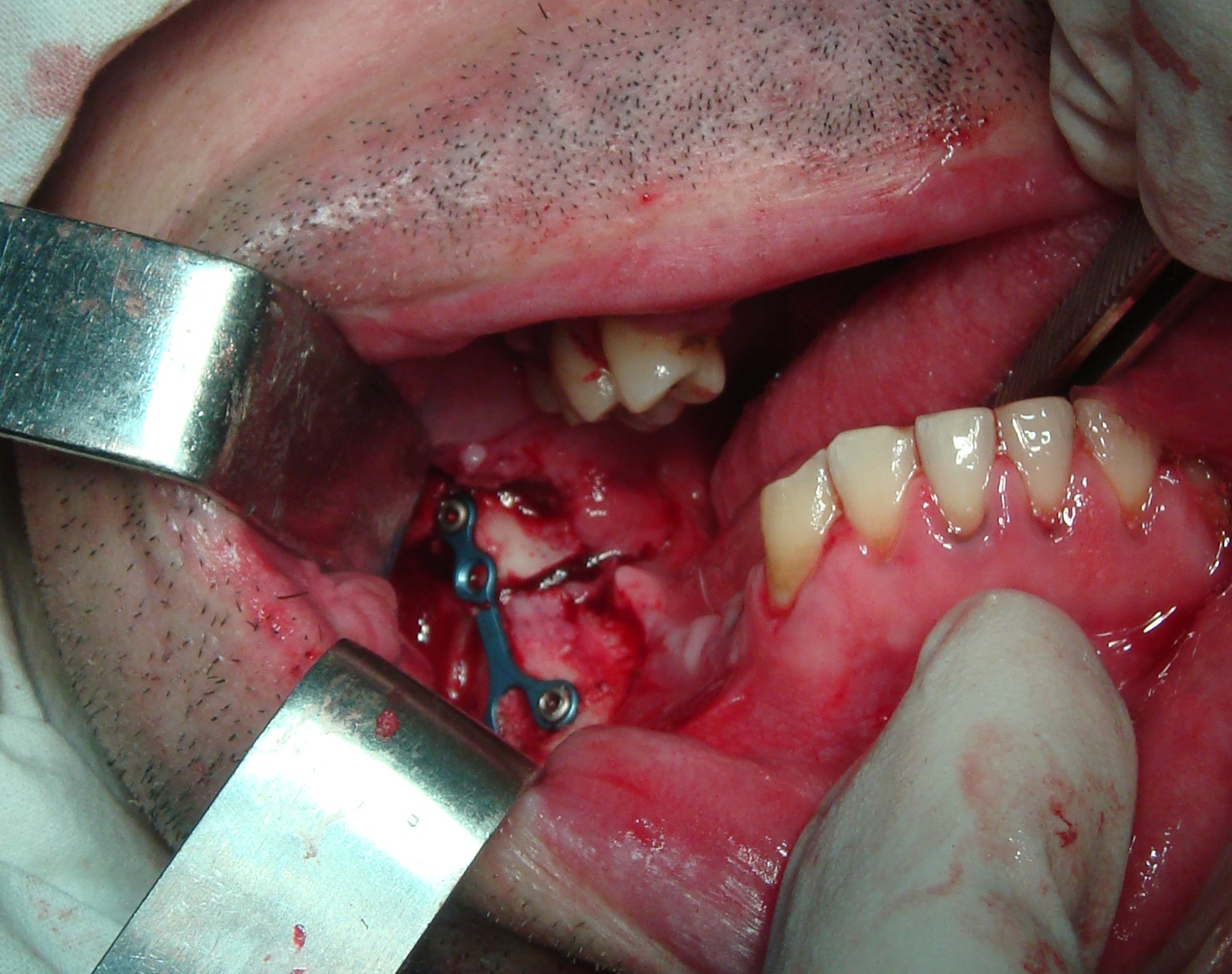
The surgery was done by I.I.F. and V.A.R. under the general anesthesia. First, parts of the lower right third molar were removed according to the indications.9 Secondly, open reduction of the mandible fragments and Y-shape titanium mini-plate fixation were performed (Fig 4). And as a last stage, four self-tapping MMF screws were inserted in the safe zones (Cornelius and Ehrenfeld, 2010)11 after drilling holes throughout just the outer cortex of the jaws. Osteosynthesis was not performed in the area of the mandible body on the left, due to the fact that the fracture in this area was without dislocation and to avoid impaired vascularization.
The next day after the operation, the bite block was made in the dental chair by I.I.F. and after consulting the prosthodontist (O.Y.M.) and providing the necessary impression materials. C-silicone impression material set was used for the bite block-splint production. The set included the base mass (Speedex putty soft, 1000 g, Coltene/Whaledent AG, Altstätten, Switzerland), universal activator (Speedex Universal Activator, 60 mL, Coltene/Whaledent AG, Altstätten, Switzerland), and corrective mass (Speedex Light Body, 140 mL, Coltene/Whaledent AG, Altstätten, Switzerland).
Stages of the C-silicone bite block-splint fabrication using two-layer technique:
-
Base mass was taken in the volume necessary to cover the alveolar processes, teeth, and teeth roots in the anterior area (with some excess for the possibility of cutting with a scalpel blade),allowing the lateral areas to be used for the intake of liquid/ground food via drinking straws.
-
Base material is mixed with an universal activator and a roller is made, which is introduced in an arc between the upper and lower alveolar processes, teeth and existing teeth roots. Next, the doctor had to use his fingers to plaster the outer surfaces of the teeth with silicone (until it had hardened) (that is, to somewhat simulate the vestibular surface with his own hands). We were guided by prosthodontic protocols for determining non-fixed bite height.
-
After hardening, the bite block-splint is removed from the oral cavity.
-
Volume surpluses and edges of the bite block are trimmed, smoothed (using surgical blade no. 10) and grooves are created in the places where the elastics pass.
-
After correction-adaptation of the block to the relief of surrounding tissues and direction/position of the elastics, the corrective mass is mixed with an universal activator, introduced bilaterally into the block-splint, inserted into the oral cavity and the patient was asked to bite.
-
Two elastics were worn immediately after insertion of the splint (Fig 5).
It is worth noting that the attending doctor (I.I.F.) initially tried to make the block-splint similar to the Port and Gunning splint in the matter of creating an opening in the anterior part of the splint. In this case, it is a through round hole. But the created hole was larger than 1 cm what significantly weakened the rigidity of the splint structure and made it weak, which is why the splint had to be refabricated. Therefore, they refused to create a hole at that moment. Also, excessively reducing the volume (external contours) of the block-splint led to the loss of its necessary stabilizing function, and such an excessively reduced volume of the block-splint also had to be refabricated. In total, two block-splints were not properly trimmed, and the third already met most of the requirements. It was used for treatment.
Perhaps it is most expedient to use a bone harvesting trephine of the appropriate diameter (~7/8 mm) to create a hole. At the same time, in our opinion, it is better not to make the diameter of the hole more than 8/9 mm, as this can significantly weaken the structure of the block-splint. However, the 7/8 mm opening is sufficient for a feeding tube to pass through and to receive liquid/ground food and liquids.
The roots of teeth no. 1.5, 1.4, 2.3, and 4.4 were not removed (1) to use them as retention (support) points for the silicone block and (2) to avoid a possible complication in the form of a dry socket, the treatment of which would require removal of the block at the stage of fracture healing. Such tooth roots as the roots of teeth 1.5, 1.4, 2.3, and 4.4 can be named as temporary additional retention points.
Comparison of the pretreatment view and anterior view on postoperative day one is presented in Figure 6.
Intermaxillary elastics were temporarily worn during the block fabrication. And immediately after its fabrication and application of the indurent gel, elastics were worn for 3 weeks. They were replaced every 7 days. Elastics were made from a Foley catheter by cutting it crosswise. On the 21st day from the moment of permanent fixation of the elastics, the elastics, block, and screws in which the mobility began to appear were removed. Healing of fracture sites was smooth, and no complaints were reported from the patient’s side.
Describing proposed intermaxillary silicone appliance we use the term bite block-splint because with closed jaws, temporary additional retention points and equators of existing teeth create a lock splint effect and opening the jaws even without rubber pulls is difficult for the patient.
Combined use of intermaxillary C-silicone bite block-splint and four MMF screws with intermaxillary rubber pulls provided adequate stabilization. Such technique can be applied in partially edentulous mandible fracture cases: (1) after the open reduction internal fixation of dislocated fracture, (2) for the conservative treatment of fracture without dislocation, and (3) in bilateral fractures and combination of open reduction internal fixation of dislocated fracture and conservative treatment of fracture without dislocation (like in the presented case).
DISCUSSION
Management of dentulous mandibular fractures can include application of completely different types of intermaxillary and MMF appliances. Like, vacuum-formed splints with bonded wire cleats for temporary intermaxillary fixation (Lloyd and colleagues, 2001),12 intraoral cortical bone screws and specially designed metal Otten hooks (also known as Ottenhaken) (Poeschl and colleagues, 2008),13 Ivy loops/eyelet wiring (Chacon and Larsen, 2004; Touré and colleagues, 2023),14,15 lingual splint (Chacon and Larsen, 2004; Balasubramanian and colleagues, 2017),14,16 Tigershtedt arch bars, Tymofieiev, 2012),17 Erich/Vasyliev arch bars (Blitz and Notarnicola, 2009; Tymofieiev, 2011),18,19 intermaxillary fixation with bra hook (Pynn and colleagues, 2022),20 Risdon cables with elastics for patients with primary and mixed dentitions (Marschall and colleagues, 2023),21 and many more.
However, the treatment of partially or totally edentulous mandibular fractures requires other tactics or their combinations. For example, for the partially edentulous mandibular fractures can be used intermaxillary transmucosal fixation by osteosynthesis miniplates (Melo and colleagues, 2012),22 the SMARTLock hybrid arch bars (Carlson and colleagues, 2017),23 pre-existing removable partial dentures as modified splint for intermaxillary fixation (Prajapati and Sathaye, 2018),24 Weber splint (Tymofieiev, 2020),25 etc.
For the totally edentulous mandibular fractures was and can be used intermaxillary transmucosal fixation by osteosynthesis miniplate (Wolfe and colleagues, 1989),26 a Gunning splint with skeletal suspension and MMF (Buchbinder, 1993),27 Port splint (Tymofieiev, 2012),17 the resin bite blocks with imbedded arch bars (i.e., Gunning splint) (Chacon and Larsen, 2004; Sharma and colleagues, 2020)14,5 and MMF, the MMF screws to fix intact complete dentures to the bone with elastics (Newaskar and colleagues, 2013),28 Gunning splint modified to complete dentures prosthesis (Shah and colleagues, 2018),4 virtually planned Gunning splints fabricated with wings and holes projected in areas of secure bone anchorage (Duran-Rodriguez and colleagues, 2022),29 and other similar techniques.
The use of silicone blocks for intermaxillary fixation has already been documented in the report by Ergün (2003).30 But in their study, it was a different type of silicon block, namely medical grade silicone block which is carved by surgeon depending on the surgical needs of the clinical situation. Such type of carved medical grade silicone block was applied as a pellet for the treatment of minor malocclusion upon the mandible condyle fracture management with a purpose to restore functional occlusion. Medical grade silicone is a flexible silicone elastomermaterial designed for implant or to reconstruct or augment cartilaginous tissue. For the same purposes, application of the pieces of rubber tube in several layers, rubber stoppers from vials for medicinal substances, etc. are described by Tymofieiev (2020).25
A-silicones (also known as polyvinyl siloxanes [PVS] or vinyl polysiloxanes [VPS]) (Rubel and colleagues, 2007; Muñoz-Viveros, 2012)31,32 and C-silicones are elastic and irreversible impression materials and typically used to replicate the structures of the oral cavity. Theoretically, both types of those silicones could also be applied for fabrication of the bite block-splint that can work in combination with MMF screws to immobilize the mandible fragments. But in this study, we analyze the application only a C-silicone material. C-silicone which was used in our case met all requirements the patient’s intraoral situation needed: Low cost of fabrication, possibility to fabricate without assistance of dental technician, and can be adapted to partially edentulous jaws and lack of occlusion. Moreover, the production of such a block splint turned out to be surprisingly fast and possible not only without the presence and help of a dental technician, but also a prosthodontist. Therefore, such blocks can be made by surgeons themselves if they have С- or A-silicone impression material and indurent gel in their office.
Qureshi and colleagues (2016) emphasized that intermaxillary fixation with MMF screws is more efficacious compared to conventional Erich arch bars in the treatment of mandible fracture.33 The types of the MMF screws and its use is perfectly described in the study by Cornelius and Ehrenfeld in 2010.11 Also, numerous and distinctive advantages of intermaxillary screws over traditional methods were highlighted in their study.11 Kim and colleagues (2022) stated that the average time required for screws fixation is 15.38 minutes,34 what is faster than arch bars fixation to the dentulous arches.
Tooth root injury caused by MMF screws placement is need to be prevented taking into account safe and danger zones for screw insertion (Ma and colleagues, 2023).35 Hartwig and colleagues in 2017, emphasized that 12.5 percent of the screws caused radiological root injuries.36
Speaking about our case, the total speed of installing MMF screws and making a C-silicone bite block-split is many times faster than fixing arch bars on the dental arches or making a Gunning splint by dental technicians.
The average period of fixation of arch bars for the consolidation of fragments of the mandible in case of bilateral fracture is 25 ± 2 days (Tymofieiev, 2011).19
Given open reduction internal fixation of the mandibular angle and non-dislocated fracture of the left mandibular body in our case, we endured intermaxillary fixation for three weeks.
However, the findings from the study by Certa and colleagues (2023) suggest that a short duration (less than two weeks) of postoperative MMF may reduce postoperative inflammatory complications following open reduction internal fixation of mandibular angle fractures.37
The elastic rubber bands need to be changed every 5–6 days (or as it stretches) (Tymofieiev, 2012).17
The technique presented by our team can be used as a new alternative to the application of the MMF screws inserted through the Gunning splints in partially edentulous cases (Chaudhary and colleagues, 2014) and to many other techniques due to a lot advantages.6
Absence of pathological effects of metal and plastic inclusions on oral tissues (Tymofieiev, 2012) are among the advantages of the combination of the silicone bite block-splint and MMF screws usage.17
Successful application only of two Otten hooks and one elastic rubber band in non-dislocated or slightly mandibular fractures (Poeschl and colleagues, 2008)13 indirectly but confirm the idea that the use of four MMF screws and two elastics which are presented in our case is more than sufficient (Roccia and colleagues, 2005).13, 38 Nevertheless, up to six MMF screws can be used in similar to our case situations.
С-silicone is the preferred choice for many dentists in Ukraine, but we can theoretically assume that A-silicone material can also be used for the silicone bite block-splint fabrication.
So, the Gunning splint has been modified numerous times from the moment of its introduction (Romm, 1986)39 and during its application by different specialists and in various intraoral circumstances (Goss and Brown, 1975; Dharaskar and colleagues, 2014; Singh and colleagues, 2017; Hwang and Ma, 2021)40–43. Juraj Halmoš (1975) described the use of an individually made plastic monoblock for fractures treatment of jaws with an incomplete number of teeth.44 The monoblock was made with a hole for food intake, attached to the teeth with the help of ligatures and the jaws were immobilized by means of extraoral traction-fixation between the parietal and the chin region.44 The silicone bite block-splint that we proposed for MMF purposes upon treatment of partially edentulous mandible fractures with a nonexistent occlusion and bite height also partially borrowed the idea from Gunning splint and somewhat resembles a Halmoš monoblock.
Critical analysis of classification system of partially edentulous spaces was performed by Ahilaand colleagues (2019).45 Potential benefits of the classification system for partial edentulism are described in the study by McGarry and colleagues (2002).46 Same benefits are similar for the classification proposed by our team (i.e., Kennedy–Kyiv Classification System) for the mandibular fractures in situation of partially edentulous arches. Among benefits are an improving professional communication between colleagues, improving the assessment of treatment complexity and insurance reimbursement according to complexity, etc.
Summarizing our report, it is worthy to note that among the advantages of such a C-silicone bite block-splint comparing to other Gunning-type splints are:
-
No need to involve a dental technician or prosthodontist.
-
Production speed.
-
Significantly reduced fabrication cost.
-
Application of the indurent gel for manufacturing of such block-splint minimize the micromovements.
-
Absence of pathological effects of plastic and metal inclusions on oral tissues.
The dimensions of the silicone bite-block in the three-dimensional plane should be minimal, at the same time, such that the movements of the lower jaw will be impossible when applying rubber traction.
It is recommended to further study the short- and long-term results of the application of the highlighted technique with C- or even A-silicone materials, different number of fracture sites and the degree of their dislocation, the duration of use of intermaxillary rubber traction in different types of fractures and different types of treatment. The safety characteristics of the C-silicone material which was used in our report are highlighted at the safety data sheets for all three components of the impression material set.47–49
Treatment of each specific fracture of the lower jaw, which is a multi-functional bone,50 is a unique challenge even for experienced doctors. This is why analyzing and understanding all possible old and new treatment modalities and combinations is so important. After all, such knowledge can make it possible to propose new methods applying the new combination of existed materials.
CONCLUSIONS
The proposed in this paper technique allows to decrease the time typically required for the Gunning splints fabrication, decrease number of the involved specialists, decrease cost of treatment, and easy for performance. With the advent and understanding of this technique, oral and maxillofacial surgeons will have in their arsenal another option for the treatment of partially edentulous mandible fractures in cases of nonexistent occlusion.
TERM OF CONSENT
Writing patient’s consent was obtained for publication the photos.
AUTHORS’ CONTRIBUTIONS
Material collection and conceptualization: Fesenko II. Data analysis and interpretation: all authors. Drafting of the manuscript: Fesenko II. Critical revision of the manuscript: all authors. Approval of the final version of the manuscript: all authors.
CONFLICT OF INTERESTS
The authors declare no conflict of interest.
FUNDINGS
No funding was received for this study.
REFERENCES (50)
-
Khan SA, Tushar, Nezam S, et al. Comparison and evaluation of linear dimensional accuracy of three elastomeric impression materials at different time intervals using vision inspection system: an in vitro study. J Int Soc Prev Community Dent 2020;10(6):736–42. https://doi.org/10.4103%2Fjispcd.JISPCD_282_20
-
Gunning TB. Treatment of fracture of the lower jaw by interdental splints. Am J Dent Sci 1868;2(4):172–9.
-
Fraser-Moodie W. Mr. Gunning and his splint. Br J Oral Surg 1969;7(2):112–5. https://doi.org/10.1016/S0007-117X(69)80006-5
-
Shah SP, Verma VB, Talkal AK, et al. Gunning splint modified to complete dentures prosthesis: a conservative management of edentulous mandibular fracture. J Clin of Diagn Res 2018;12(7):ZD01–ZD03. https://www.doi.org/10.7860/JCDR/2018/32745/11714
-
Sharma B, Sharma P, Goswami R, et al. Construction of a gunning splint; case report on the handling of mandibular fractures in edentulous patients. Indian J Dent Sci 2020;12:36–9. https://doi.org/10.4103/IJDS.IJDS_92_19
-
Chaudhary Z, Sharma R, Krishnan S. Maxillo mandibular fixation in edentulous scenarios: combined MMF screws and Gunning splints. J Maxillofac Oral Surg 2014;13(2):213–4. https://doi.org/10.1007/s12663-013-0481-z
-
Nosyr OV, Fesenko II, Khrulenko SI. Mandibular fractures: pre-operative panoramic radiography and duplication sign patterns. J Diagn Treat Oral Maxillofac Pathol 2021;5(5):57–66. https://doi.org/10.23999/j.dtomp.2021.5.1
-
Passi D, Malkunje L, Atri M, et al. Newer proposed classification of mandibular fractures: a critical review with recent updates. Ann Med Health Sci Res 2017;7:314–8.
-
Şakar O. Classification of partially edentulous arches. In: Şakar O, editor. Removable partial dentures. Cham: Springer; 2016:17–21. https://doi.org/10.1007/978-3-319-20556-4_3
-
Tymofieiev OO, Fesenko II, Tymofieiev OO. Condition of the teeth in fracture gap of the mandible. J Diagn Treat Oral Maxillofac Pathol 2017;1(1):41−53. https://doi.org/10.23999/j.dtomp.2017.1.6
-
Cornelius CP, Ehrenfeld M. The use of MMF screws: surgical technique, indications, contraindications, and common problems in review of the literature. Craniomaxillofac Trauma Reconstr 2010;3:55–58. https://doi.org/10.1055/s-0030-1254376
-
Lloyd T, Nightingale C, Edler R. The use of vacuum-formed splints for temporary intermaxillary fixation in the management of unilateral condylar fractures. Br J Oral Maxillofac Surg 2001;39(4):301–3. https://doi.org/10.1054/bjom.2001.0649
-
Poeschl PW, Ploder O, Seemann R, Poeschl E. Maxillomandibular fixation using intraoral cortical bone screws and specially designed metal hooks (Ottenhaken) in the conservative treatment of mandibular fractures. J Oral Maxillofac Surg 2008;66:336–41. https://doi.org/10.1016/j.joms.2007.06.671
-
Chacon GE, Larsen PE. Principles of management of mandibular fractures. In: Miloro, editor. Peterson’s principles of oral and maxillofacial surgery. 2nd edition. Hamilton: BC Decker Inc; 2004:401–33.
-
Touré LB, Ongoiba O, Kasssogué D, et al. Eyelet wiring in closed reduction in the treatment of mandibular fracture: a case report. East African Scholars J Med Surg 2023;5(9):156–7.
-
Balasubramanian S, Panneerselvam E, Sharma AR, et al. Lingual splint for sagittal fractures of mandible; An effective adjunct to contemporary osteosynthesis: a case series with review of literature. Craniomaxillofac Trauma Reconstr Open 2017;1:e9–e14. https://doi.org/10.1055/s-0037-1603578
-
Tymofieiev OO. Manual of oral and maxillofacial surgery (in Russian). 5th ed. Kyiv: Chervona Ruta-Turs; 2012:456–504.
-
Blitz M, Notarnicola K. Closed reduction of the mandibular fracture. Atlas Oral Maxillofac Surg Clin North Am2009;17(1):1–13. https://doi.org/10.1016/j.cxom.2008.10.002
-
Tymofieiev OO. Maxillofacial surgery (in Ukrainian). Kyiv: Medicine, All-Ukrainian Specialized Publishing House; 2011:370–455.
-
Pynn BR, Mauro F, Nish IA. Intermaxillary fixation with bra hooks. Br J Oral Maxillofac Surg 2022;60(6):852–4. https://doi.org/10.1016/j.bjoms.2021.12.007
-
Marschall JS, Barnes S, Kushner GM. Intermaxillary Fixation in the Primary and Mixed Dentition. Oral Maxillofac Surg Clin North Am 2023;35(4):521–7. https://doi.org/10.1016/j.coms.2023.04.002
-
Melo AR, do Amaral MF, de Santana Santos T, et al. Conservative treatment of comminuted mandibular fracture involving maxillomandibular fixation with miniplates. J Craniofac Surg 2012;23(3):893–5. https://doi.org/10.1097/SCS.0b013e31824e2528
-
Carlson AR, Shammas RL, Allori AC, Powers DB. A technique for reduction of edentulous fractures using dentures and SMARTLock hybrid fixation system. Plast Reconstr Surg Glob Open 2017;5(9):e1473. https://doi.org/10.1097/gox.0000000000001473
-
Prajapati A, Sathaye S. Use of pre-existing removable partial dentures as modified splint for intermaxillary fixation in case of guardsman fracture: a case report. Int J Recent Scie Res 2018;9(10)(D):29320–29323.
-
Tymofieiev OO. Maxillofacial surgery and surgical dentistry (in Russian). In two volumes. Volume 1. Kyiv: Medicine, All-Ukrainian Specialized Publishing House; 2020:813–86.
-
Wolfe SA, Lovaas M, McCafferty LR. Use of a miniplate to provide intermaxillary fixation in the edentulous patient. J Craniomaxillofac Surg 1989;17(1):31–3. https://doi.org/10.1016/s1010-5182(89)80124-6
-
Buchbinder D. Treatment of fractures of the edentulous mandible, 1943 to 1993: a review of the literature. J Oral Maxillofac Surg 1993;51(11):1174–80. https://doi.org/10.1016/s0278-2391(10)80285-x
-
Newaskar V, Agrawal D, Idrees F, Patel P. Simple way of fixing a Gunning-type splint to the bone using intermaxillary fixation screws: technical note. Br J Oral Maxillofac Surg 2013;51(4):e59–e60. https://doi.org/10.1016/j.bjoms.2012.04.075
-
Duran-Rodriguez G, Gómez-Delgado A, López JP. Management of bilateral condylar fractures in an edentulous patient with atrophic mandible using CADCAM technology. J Maxillofac Oral Surg 2022;21(1):124–8. https://doi.org/10.1007/s12663-021-01652-8
-
Ergün SS. Use of silicone block as a pellet in the treatment of minor malocclusion. Ann Plast Surg2003;51(2):225–6. https://doi.org/10.1097/01.SAP.0000063744.68992.20
-
Rubel BS. Impression materials: a comparative review of impression materials most commonly used in restorative dentistry. Dent Clin North Am 2007;51(3):629–vi. https://doi.org/10.1016/j.cden.2007.03.006
-
Muñoz-Viveros CA. Impression materials. In: Freedman G, editor. Contemporary esthetic dentistry. St. Louis, Missouri: Elsevier Mosby; 2012:33–50. https://doi.org/10.1016/B978-0-323-06895-6.00002-5
-
Qureshi AA, Reddy UK, Warad NM, et al. Intermaxillary fixation screws versus Erich arch bars in mandibular fractures: a comparative study and review of literature. Ann Maxillofac Surg 2016;6(1):25–30. https://doi.org/10.4103/2231-0746.186129
-
Kim YG, Yoon SH, Oh JW, et al. Comparison of intermaxillary fixation techniques for mandibular fractures with focus on patient experience. Arch Craniofac Surg 2022;23(1):23–8. https://doi.org/10.7181%2Facfs.2021.00549
-
Ma H, Liu H, Shen Y. Tooth root injury caused by intermaxillary fixation screw placement. Asian J Surg. 2023;46(12):5822-5823. https://doi.org/10.1016/j.asjsur.2023.08.152
-
Hartwig S, Boettner A, Doll C, et al. Drill-related root injury caused by intraoperative intermaxillary fixation: an analysis of 1067 screw applications. Dent Traumatol 2017;33(1):45e50.
-
Certa M, Chapple AG, Khalifa A, Christensen BJ. Does a short period of maxillomandibular fixation decrease complications in open reduction internal fixation of mandibular angle fractures? J Oral Maxillofac Surg2023;81(4):406–12.
-
Roccia F, Tavolaccini A, Dell'Acqua A, Fasolis M. An audit of mandibular fractures treated by intermaxillary fixation using intraoral cortical bone screws. J Craniomaxillofac Surg 2005;33(4):251–4. https://doi.org/10.1016/j.jcms.2005.02.005
-
Romm S. Thomas Brian Gunning and his splint. Plast Reconstr Surg 1986;78(2):252–8. https://doi.org/10.1097/00006534-198608000-00024
-
Goss AN, Brown RO. An improved Gunning splint. J Prosthet Dent 1975;33(5):562–6. https://doi.org/10.1016/s0022-3913(75)80171-5
-
Dharaskar S, Athavale S, Kakade D. Use of gunning splint for the treatment of edentulous mandibular fracture: a case report. J Indian Prosthodont Soc 2014;14(4):415–8. https://doi.org/10.1007/s13191-013-0294-2
-
Singh G, Sahni V R, Kaur D, et al. Customized gunning splint for para sagittal palatal split with right alveolar fracture - a case report. IP Ann Prosthodont Restor Dent 2017;3(2):85–7.
-
Hwang K, Ma SH. Use of a monoblock gunning splint in a bilateral condylar fracture in an edentulous patient. J Craniofac Surg 2021;32(3):e235–e238. https://doi.org/10.1097/SCS.0000000000006963
-
Halmoš J. Traumatology of the maxillofacial skeleton (in Russian. Translation from Slovak). Bratislava: Veda, Publishing House of the Slovak Academia of Science; 1975;113–48.
-
Ahila SC, Suganya S, Muthukumar B. Critical analysis of classification system of partially edentulous spaces: a literature review. Indian J Multidiscip Dent 2019;9:49–57. https://doi.org/10.4103/ijmd.ijmd_43_18
-
McGarry TJ, Nimmo A, Skiba JF, et al. Classification system for partial edentulism. J Prosthodont2002;11(3):181–93.
-
Safety data sheet: Speedex putty soft. COLTENE/Whaledent AG. Revision date: 22.10.2020. Print date: 27.10.2020.
-
Safety data sheet: Speedex universal activator. COLTENE/Whaledent AG. Revision date: 17.06.2015. Print date: 25.06.2015.
-
Safety data sheet: Speedex light body. COLTENE/Whaledent AG. Revision date: 22.10.2020. Print date: 27.10.2020.
-
Pham TD, Holmes SB, Patel M, Coulthard P. Features and networks of the mandible on computed tomography. R Soc Open Sci 2024;11:231166. https://doi.org/10.1098/rsos.231166